
Give Up All Your Favorite Foods With Diabetes? Not Necessarily So, Says City Of Hope Dietitian
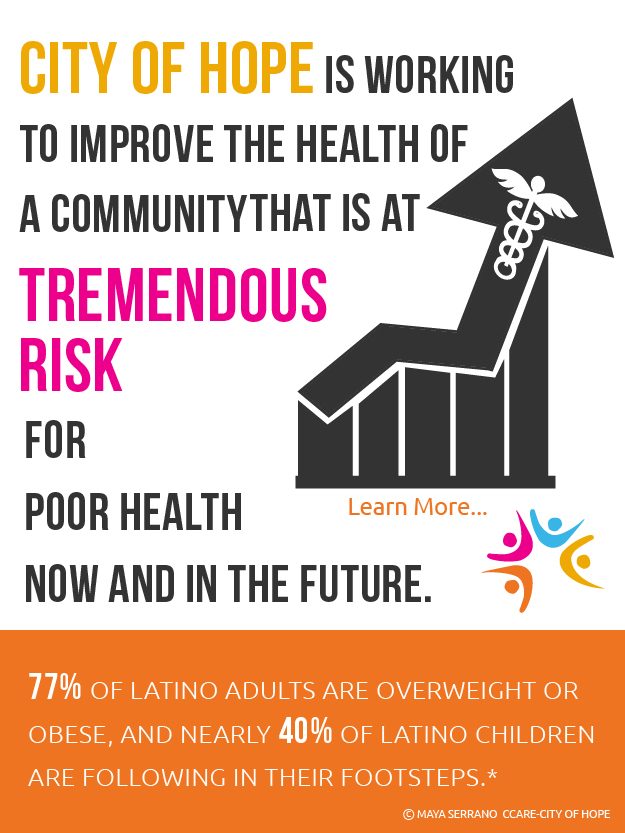
07/15/2015 03:39PM | 7353 viewsA diagnosis of diabetes typically means altering one’s diet to make it healthier, and more successfully manage the disease.
But it’s a scary thought for many Hispanics and Latinos, who often assume they’ll need to give up everything they love and radically change their eating style to stay well.
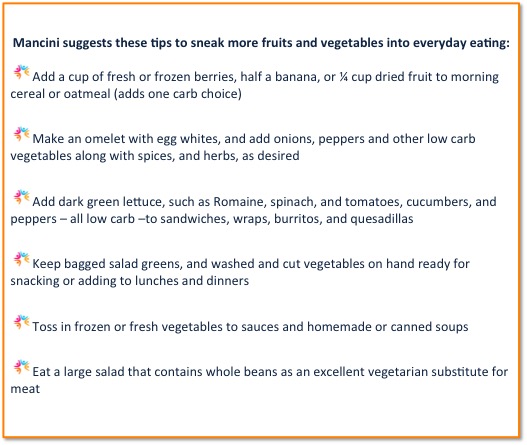
Not so, says Peggy Mancini, a Registered Dietitian (R.D.) and Certified Diabetes Educator (C.D.E.) who counsels Type 1 and Type 2 diabetes patients at City of Hope near Los Angeles.
“I don’t try to drastically change their diet,” she says. “With diabetes, people need to be more concerned about balance.”
When working with Latino and other diabetes patients, Mancini carefully examines each patient’s diet to make minor modifications, focusing on adjusting quantity and portion size. She also explains the choices they have to help them achieve more dietary balance.
Manage Carbs Effectively
Controlling blood sugar – especially by managing carbohydrates eaten – is key to achieving that balance and managing diabetes successfully, Mancini says. Carbohydrates include breads and tortillas, milk and milk products, fruits, beans, lentils, rice, sweets and other sugary foods, and affect blood sugar more than proteins and fats.
People living with diabetes must learn to make “carb choices,” says Mancini, who teaches patients to count their carbohydrates. One carb “choice provides 15 grams of carbohydrate, such as ¼ cup cooked beans or 1/3 cup cooked rice. Women typically need about three or four carb choices at each meal. Most men require about five to six carb choices or 75 – 90 grams of carbohydrate per meal. Snacks provide one to two carb choices. Diets should also contain low carbohydrate, protein-rich foods such as chicken, fish, meat; low carbohydrate vegetables, including broccoli, lettuce, peppers; and healthy fats (olive oil, nuts, peanut butter, avocado).
Rather than making drastic changes, Mancini might suggest that someone who typically consumes four or five tortillas at dinner trim that number to two, or make another change to reduce carbohydrates. She might suggest corn tortillas instead of flour, for a more whole grain approach.
“They have choices, too,” Mancini says. “If they don’t eat rice, for example, they can have more beans. If they want to make a cheese quesadilla with a large tortilla that includes 45 grams of carbohydrates, and they are limited to 45 grams of carbohydrates for a meal, then everything else in the meal needs to be from a low-carb source.” That can include chicken or fish, low carb vegetables, or healthy fats, such as avocado and nuts.
“So they can pick and choose,” she says.
There’s a lot to remember, but over time, making healthier selections can become an easy mental habit.
Build a Healthy Plate
As a patient’s diet adjusts, the plate may also look a little different, too.
Start with a small portion of chicken, fish or other lean protein the size of a deck of cards or the palm of your hand, Mancini says. That should fill about ¼ of the plate. Another ¼ should include fruit or healthy starches, such as whole beans or brown rice. Devote the remaining plate space to salad and vegetables. Wash it all down with water or other low or no-calorie drinks. Because obesity is a key risk factor for Type 2 Diabetes, following this rule will not only help keep your weight in check, but also help prevent family members from developing the disease, she says.
Another way to eat healthier – and learn correct portion sizes, includes incorporating Healthy Choice, or Weight Watchers Smart Ones frozen meals. These options are controlled for calories, nutrients and carbohydrates. They can be used to replace the occasional meal, but also help diabetics learn correct portion size when cooking for themselves or dining out, Mancini says.
“And the food that’s good for someone with diabetes, is also good for the whole family,” she notes, “It doesn’t mean forcing a special diet on your loved ones.”
Include the Occasional Sweet
Managing sugar intake is important, as well, with diabetes. But it doesn’t necessarily mean giving up the occasional after-dinner delight.
People with diabetes can potentially eat ice cream, cake, cookies and other sweets in portions within their carbohydrate goal, based on their individual circumstances, Mancini says.
“It depends on the rest of a person’s diet,” Mancini says. “Are they typically eating a healthy diet? Are the sweets used on occasion and not playing a large part of their diet or crowding out healthier food choices? Is their blood glucose (sugar) well controlled?”
Join Programs that Promote Exercise and Weight Control
In addition to working with a dietitian, doctors often recommend that new patients attend education programs to learn to better manage their disease and control weight.
Topics typically include insulin use, diet and exercise, stress management, and prevention of long-term complications. In addition, City of Hope near Los Angeles also offers the Diabetes and Cardiovascular Risk Reduction program for people more than 30 pounds overweight. Throughout the yearlong outreach, patients meet weekly to learn about nutrition and behavior modification. They gain skills to make lifestyle changes and keep their weight in check. Success in programs such as these often means diabetics no longer need medication.
“I recall one Hispanic gentleman who was absolutely horrified that he was being diagnosed with diabetes,” Mancini says. “He clenched his fist on the table and firmly stated ‘I will NOT have this disease’. He lost 17 pounds by making lifestyle changes with his diet and increasing exercise. His blood glucose levels improved to the point that medication was not required.”
Mancini says patients can also join weight-loss programs, such as Weight Watchers and Jenny Craig, to achieve some of the same benefits.
Tap Technology to Support The Journey
Mancini encourages people living with diabetes to rely on tools around them to help manage weight.
With a smart phone or tablet, users can tap into the many online apps that track eating, calories and exercise. MyFitnessPal, for example, allows users to enter their target weight and choose how much they’d like to lose per week, then provides a daily calorie goal. As users input meals into the app each day, it tallies the calories and provides detailed nutritional breakdowns. Other calorie counting apps include ControlMyWeight, Lose It! and Noom Coach. Some apps can also be “paired” with fitness tracker bracelets such as Fitbit and Jawbone “Up” to count daily steps and exercise – and reveal actual daily calories burned.
Some of these aides also offer online versions, such as MyFitnessPal and CalorieKing.com. Many apps also allow you to connect with friends, family or a larger online community for greater support.
“Online programs have been noted to be highly successful,” Mancini says. “Receiving support from others can improve success whether you’re online, or not. It’s good to have a friend who can encourage you to exercise, or a family member who brings healthy food into the house.”
By managing their disease more closely and taking the dietitian’s advice, people living with diabetes can continue eating the foods they love, while making smarter decisions that can reduce weight and improve overall health.









Post your Comment
Please login or sign up to comment
Comments